Risk factors for postoperative infection after combat related head injuries
DOI:
https://doi.org/10.55005/sjns.v1i1.3Keywords:
combat injury, head, brain, tbi, infection, outcomeAbstract
Introduction
The prevalence of penetrating head injuries (PBI) has increased during the latest wars making up to 37,4% of all injuries (1,2) Microbiology of modern war wounds is unique for each military conflict depending on the climatic and geographical features of the theater of combat (3,4).
Material and methods:
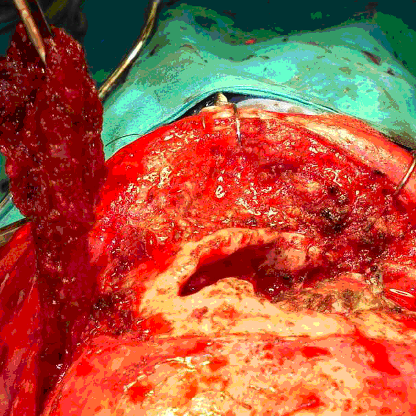
286 patients were operatively treated after penetrating combat injury in our institution between 1991-1999. Based on the inclusion criteria: combat-related cranial injury and absence of severe abdominal or chest combat injuries, as well as their ability to report for a follow-up exam led to the inclusion of 202 patients. Initial surgical treatment included removal of devitalized soft tissue and bone fragments with craniectomy, removal of devitalized brain tissue, easily accessible intracerebral bone and metal fragments and intracranial hemathoma. All patients received the same standardized postoperative care with triple antibiotics.
Results Infection occurred in 36 patients (17,82%). In vast majority of the cases infection occurred in the form of brain abscess 31 (86.11%), in 4 cases as meningitis (11.1%) and in 1 case as osteomyelitis and epidural infection (2.78%). Retained metal and bone fragments and postoperative liquorrhea have significant influences on occurrence of postoperative infection. Conclusion Postoperative infection considerably increases long term functional outcome. Using advantages of minimally invasive surgical technique, neuronavigation or intraoperative imaging for removal of retained foreign bodies can reduce risk for postoperative infection with minimal risk of additional neurologic deficit. Autograft is preferable option for dural reconstruction in combat related head injuries.References
MacGregor AJ, Dougherty AL, Galarneau MR. Injury-specific correlates of combat-related traumatic brain injury in Operation Iraqi Freedom. J Head Trauma Rehabil. 2011;26(4):312-318. doi: 10.1097/HTR.0b013e3181e94404
Gizatullin SK, Stanishevskiy AV, Svistov DV. Combat gunshot skull and brain injuries. Zh Vopr Neirokhir Im N N Burdenko. 2021;85(5):124-131. doi: 10.17116/neiro202185051124
Valentine KP, Viacheslav KM. Bacterial flora of combat wounds from eastern Ukraine and time-specified changes of bacterial recovery during treatment in Ukrainian military hospital. BMC Res Notes. 2017;10(1):152. Published 2017 Apr 7. doi: 10.1186/s13104-017-2481-4
Murray CK, Roop SA, Hospenthal DR, et al. Bacteriology of war wounds at the time of injury. Mil Med. 2006;171(9):826-829. doi: 10.7205/milmed.171.9.826
Pringle C, Bailey M, Bukhari S, et al. Manchester Arena Attack: management of paediatric penetrating brain injuries. Br J Neurosurg. 2021;35(1):103-111. doi: 10.1080/02688697.2020.1787339
Marquardt G, Schick U, Möller-Hartmann W. Brain abscess decades after a penetrating shrapnel injury. Br J Neurosurg. 2000;14(3):246-248. doi:10.1080/026886900408450
Milton J, Rugino A, Narayan K, Karas C, Awuor V. A Case-Based Review of the Management of Penetrating Brain Trauma. Cureus. 2017;9(6):e1342. Published 2017 Jun 12. doi: 10.7759/cureus.1342
Amirjamshidi A, Abbassioun K, Rahmat H. Minimal debridement or simple wound closure as the only surgical treatment in war victims with low-velocity penetrating head injuries. Indications and management protocol based upon more than 8 years follow-up of 99 cases from Iran-Iraq conflict. Surg Neurol. 2003;60(2):105-111. doi: 10.1016/s0090-3019(03)00358-6
Bhatoe HS. Missile injuries of the anterior skull base. Skull Base. 2004;14(1):1-8. doi: 10.1055/s-2004-821351
Darwazeh R, Darwazeh M, Sbeih I, Yan Y, Wang J, Sun X. Traumatic Brain Injury Caused by Missile Wounds in the North of Palestine: A Single Institution's Experience with 520 Consecutive Civilian Patients. World Neurosurg. 2018;116:e329-e339. doi: 10.1016/j.wneu.2018.04.202
Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011;4(3):395-402. doi: 10.4103/0974-2700.83871
Esposito, D P. Walker, J B. Contemporary Management of Penetrating Brain Injury, Neurosurgery Q. 2009;19(4): 249-254
doi: 10.1097/WNQ.0b013e3181bd1d53
Chaudhri KA, Choudhury AR, al Moutaery KR, Cybulski GR. Penetrating craniocerebral shrapnel injuries during "Operation Desert Storm": early results of a conservative surgical treatment. Acta Neurochir (Wien). 1994;126(2-4):120-123. doi: 10.1007/BF01476420
Surgical management of penetrating brain injury. J Trauma. 2001;51(2 Suppl):S16-S25.
Hammon WM. Analysis of 2187 consecutive penetrating wounds of the brain from Vietnam. J Neurosurg. 1971;34(2 Pt 1):127-131. doi: 10.3171/jns.1971.34.2part1.0127
Salazar AM, Jabbari B, Vance SC, Grafman J, Amin D, Dillon JD. Epilepsy after penetrating head injury. I. Clinical correlates: a report of the Vietnam Head Injury Study. Neurology. 1985;35(10):1406-1414. doi: 10.1212/wnl.35.10.1406
Management of cerebrospinal fluid leaks. J Trauma. 2001;51:S29–33.
Meirowsky AM, Caveness WF, Dillon JD, et al. Cerebrospinal fluid fistulas complicating missile wounds of the brain. J Neurosurg. 1981;54(1):44-48. doi: 10.3171/jns.1981.54.1.0044
Gönül E, Baysefer A, Kahraman S, et al. Causes of infections and management results in penetrating craniocerebral injuries. Neurosurg Rev. 1997;20(3):177-181. doi: 10.1007/BF01105561
Chaudhri KA, Choudhury AR, al Moutaery KR, Cybulski GR. Penetrating craniocerebral shrapnel injuries during "Operation Desert Storm": early results of a conservative surgical treatment. Acta Neurochir (Wien). 1994;126(2-4):120-123. doi: 10.1007/BF01476420
Levi L, Borovich B, Guilburd JN, et al. Wartime neurosurgical experience in Lebanon, 1982-85. I: Penetrating craniocerebral injuries. Isr J Med Sci. 1990;26(10):548-554.
Aarabi B, Taghipour M, Alibaii E, Kamgarpour A. Central nervous system infections after military missile head wounds. Neurosurgery. 1998;42(3):500-509. doi: 10.1097/00006123-199803000-00014
Swain SK, Arora RK, Mittal RS. Migrating Souvenir Bullet: The Management Dilemma. Ann Neurosci. 2021;28(1-2):79-81. doi: 10.1177/0972753120966495
Schulz C, Woerner U, Luelsdorf P. Image-guided neurosurgery for secondary operative removal of projectiles after missile injury of the brain. Surg Neurol. 2008;69(4):364-368. doi: 10.1016/j.surneu.2006.11.058
Splavski B, Vranković D, Saftić R, Muzević D, Kosuta M, Gmajnić R. Clinical predictors correlated to outcome of war missile penetrating brain injury. Acta Med Croatica. 2006;60(4):369-373.
Aarabi B. Comparative study of bacteriological contamination between primary and secondary exploration of missile head wounds. Neurosurgery. 1987;20(4):610-616. doi:10.1227/00006123-198704000-00018
Neal CJ, Ling GS, Ecklund JM. (2005) Management of Ballistic Trauma to the Head. In: Mahoney PF, Ryan JM, Brooks AJ, William Schwab C. (eds) Ballistic Trauma. Springer, London. 2005:325-347. doi: 10.1007/1-84628-060-5
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Goran Pavlićević

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain copyright of their work, with first publication rights granted to the publisher.