Neurosurgical service during COVID-19 pandemics in Ljubljana, Slovenia - lessons learned
DOI:
https://doi.org/10.55005/v3i1.4Keywords:
COVID-19, neurosurgery, patient management, antivirus protocol, pandemic measures, LjubljanaAbstract
Introduction: The novel coronavirus disease 2019 (COVID-19) became an important and urgent threat to global health. In Slovenia, the COVID-19 struck the health system immensely. Neurosurgery experienced difficulties, not only in regular, elective surgeries, but also during emergency situations.
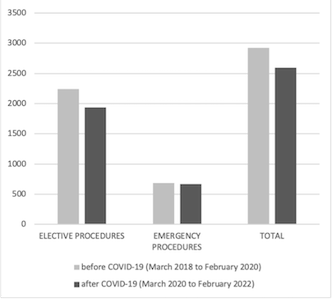
Methods: In the article, we analyse and compare the number of elective and emergency neurosurgical procedures during the time of the pandemic (from March 2018 to February 2020) and describe our protocol in the management of neurosurgical patients in the Medical Centre in Ljubljana, Slovenia.
Results: There were 2597 patients treated surgically, including 1932 emergency patients and 665 emergency patients. Overall, we recorded an 11.2% drop in all neurosurgical procedures in two years after COVID-19 was declared compared to two years before. Elective procedures decreased by 13.9%, mostly on account of spinal pathology procedures (245, 23.5%), functional neurosurgical procedures (37 cases, 24.7%), endonasal endoscopy procedures (11, 12.8%), and brain lesions (31, 4.8%).
Conclusion: COVID-19 had a vast impact on the healthcare system in Slovenia, including on neurosurgery. New and improved strategies to maintain neurosurgical practice during public health emergencies are necessary for the neurosurgical service and healthcare system to run smoothly in the long term and prevent disruptions during future pandemics.
References
Haidar MA, Shakkour Z, Reslan MA, Al-Haj N, Chamoun P, Habashy K, et al. SARS-CoV-2 involvement in central nervous system tissue damage. Neural Regen Res. 2022;17(6):1228-1239. doi: 10.4103/1673-5374.327323.
Peacock WF, Soto-Ruiz KM, House SL, Cannon CM, Headden G, Tiffany B, et al. Utility of COVID-19 antigen testing in the emergency department. J Am Coll Emerg Physicians Open. 2022;3(1):e12605. doi: 10.1002/emp2.12605.
Chams N, Chams S, Badran R, Shams A, Araji A, Raad M, et al. COVID-19: A Multidisciplinary Review. Front Public Health. 2020;8:383. doi: 10.3389/fpubh.2020.00383.
Murta V, Villarreal A, Ramos AJ. Severe Acute Respiratory Syndrome Coronavirus 2 Impact on the Central Nervous System: Are Astrocytes and Microglia Main Players or Merely Bystanders? ASN Neuro. 2020;12:1759091420954960. doi: 10.1177/1759091420954960.
World Health Organization. WHO Coronavirus (COVID-19) Dashboard (internet). 2022 August (cited 2022 August 24). Available at: https://covid19.who.int (Accessed 22. 11. 2021)
Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L, et al. Factors Associated With Surgical Mortality and Complications Among Patients With and Without Coronavirus Disease 2019 (COVID-19) in Italy. JAMA Surg. 2020;155(8):691-702. doi: 10.1001/jamasurg.2020.2713.
Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open. 2020;3(6):e2012270. doi: 10.1001/jamanetworkopen.2020.12270.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187-96. doi: 10.1097/SLA.0b013e3181b13ca2.
Leira EC, Russman AN, Biller J, Brown DL, Bushnell CD, Caso V, et al. Preserving stroke care during the COVID-19 pandemic: Potential issues and solutions. Neurology. 2020;95(3):124-133. doi: 10.1212/WNL.0000000000009713.
Arteaga AS, Aguilar LT, González JT, Boza AS, Muñoz-Cruzado VD, Ciuró FP, et al. Impact of frailty in surgical emergencies. A comparison of four frailty scales. Eur J Trauma Emerg Surg. 2021;47(5):1613-1619. doi: 10.1007/s00068-020-01314-3.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489-95. doi: 10.1503/cmaj.050051.
NIJZ Koronavirus. Available at: https://www.nijz.si/sl/koronavirus-2019-ncov (Accessed 18. 11. 2021).
Olson S, Honeybul S, Rosenfeld JV. Considering Futility of Care Decisions in Neurosurgical Practice. World Neurosurg. 2021;156:120-124. doi: 10.1016/j.wneu.2021.09.078.
Jaswaney R, Davis A, Cadigan RJ, Waltz M, Brassfield ER, Forcier B, et al. Hospital Policies During COVID-19: An Analysis of Visitor Restrictions. J Public Health Manag Pract. 2022;28(1):E299-E306. doi: 10.1097/PHH.0000000000001320.
Nejadghaderi SA, Saghazadeh A, Rezaei N. Health Care Policies and COVID-19 Prevalence: Is There Any Association? Int J Health Serv. 2022;52(1):9-22. doi: 10.1177/0020731421993940.
Agyemang K, Rose A, Baig S, Al Salloum L, Osman AA, Steckler F, et al. Neurosurgery in octogenarians during the COVID-19 pandemic: Results from a tertiary care trauma centre. Interdiscip Neurosurg. 2021;26:101357. doi: 10.1016/j.inat.2021.101357.
Sander C, Dercks NV, Fehrenbach MK, Wende T, Stehr S, Winkler D, et al. Neurosurgical Care during the COVID-19 Pandemic in Central Germany: A Retrospective Single Center Study of the Second Wave. Int J Environ Res Public Health. 2021;18(22):12034. doi: 10.3390/ijerph182212034.
Ozoner B, Gungor A, Hasanov T, Toktas ZO, Kilic T. Neurosurgical Practice During Coronavirus Disease 2019 (COVID-19) Pandemic. World Neurosurg. 2020;140:198-207. doi: 10.1016/j.wneu.2020.05.195.
Panciani PP, Saraceno G, Zanin L, Renisi G, Signorini L, Fontanella MM. Letter: COVID-19 Infection Affects Surgical Outcome of Chronic Subdural Hematoma. Neurosurgery. 2020;87(2):E167-E171. doi: 10.1093/neuros/nyaa140.
O'Dwyer MJ, Owen HC, Torrance HD. The perioperative immune response. Curr Opin Crit Care. 2015;21(4):336-42. doi: 10.1097/MCC.0000000000000213.
Fontanella MM, De Maria L, Zanin L, Saraceno G, Terzi di Bergamo L, Servadei F, Chaurasia B, Olivi A, Vajkoczy P, Schaller K, Cappabianca P, Doglietto F. Neurosurgical Practice During the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Pandemic: A Worldwide Survey. World Neurosurg. 2020;139:e818-e826.
Berry G, Parsons A, Morgan M, Rickert J, Cho H. A review of methods to reduce the probability of the airborne spread of COVID-19 in ventilation systems and enclosed spaces. Environ Res. 2022;203:111765. doi: 10.1016/j.envres.2021.111765.
Malhotra N., Joshi M., Datta R., Bajwa S.J., Mehdiratta L. Indian Society of Anaesthesiologists Advisory and Position Statement regarding COVID-19. Indian J Anaesth. 2020;64:259-263.
Matava C.T., Kovatsis P.G., Summers J.L. Pediatric airway management in COVID-19 patients—consensus guidelines from the Society for Pediatric Anesthesia's pediatric difficult intubation collaborative and the Canadian Pediatric Anesthesia Society. Anesth Analg. 2020;131:61-73.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Matic Munda, Tomaz Velnar, Borut Prestor, Tilen Zele, Peter Spazzapan, Bostjan Matos, Natasa Kos, Mitja Benedicic, Arne Jeglic, Igor Tekavcic, Andrej Porcnik, Roman Bosnjak

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain copyright of their work, with first publication rights granted to the publisher.